Heartstrings and Healing: The Emotional Impact of Cardiac ICU Travel Nursing
The emotional challenges faced by cardiac ICU travel nurses are profound. These professionals often deal with life-and-death situations, navigating the medical needs of patients who are critically ill while also supporting their families through devastating times. The pressure to provide high-quality care can be overwhelming, leading to stress, anxiety, and even burnout. For instance, during a shift, a travel nurse might be responsible for monitoring multiple patients, each with distinct and severe conditions. The nurse must remain vigilant, making quick decisions that could mean the difference between life and death. This constant state of alertness can lead to emotional fatigue. According to a recent study published in the Journal of Nursing Scholarship, nearly 40% of ICU nurses report symptoms of emotional exhaustion, a statistic that underscores the need for effective coping strategies.
The Weight of Responsibility
Cardiac ICU travel nurses not only face the burden of their patients' health, but they also carry the emotional weight of their families' fears and hopes. Each day brings the potential for both devastating news and miraculous recoveries. The emotional toll of witnessing patients in their most vulnerable states can leave lasting impressions on nurses, often resulting in what is commonly referred to as "compassion fatigue."
Personal Anecdotes: The Dual Nature of Care
Many cardiac ICU travel nurses share experiences that reflect both the emotional weight of their roles and the profound rewards of their work. For example, Sarah, a travel nurse with over five years of experience, recounts a particularly challenging case involving a young patient recovering from a heart transplant. “Every day was a roller coaster,” she recalls. “There were moments of despair when the patient would take a turn for the worse, but then there were moments of sheer joy when we celebrated small victories. It’s a unique blend of emotions that you learn to navigate.” Such experiences highlight the dual nature of care in the cardiac ICU. While the stakes are high, the nurse's ability to connect with patients and their families can also lead to incredibly rewarding moments. Celebrating a patient’s recovery or comforting a family during a difficult time can reinforce a nurse’s sense of purpose, providing motivation to overcome the emotional challenges inherent in the role.
Strategies for Self-Care and Mental Health Support
To manage the intense emotional demands of their work, cardiac ICU travel nurses must prioritize self-care and mental health. Here are some effective strategies: 1. Peer Support: Building a network of fellow nurses can provide a vital support system. Sharing experiences and strategies for coping with stress can foster a sense of camaraderie and understanding. Many travel nurses find solace in connecting with others who understand the unique challenges they face. 2. Mindfulness and Stress Reduction Techniques: Practices such as meditation, yoga, and deep-breathing exercises can help nurses manage anxiety and promote emotional well-being, allowing them to remain focused and calm in high-pressure situations. Mindfulness techniques, in particular, have been shown to improve emotional resilience among healthcare professionals. 3. Professional Counseling: Engaging with mental health professionals can provide nurses with tools to process the emotional toll of their work. Many healthcare organizations offer counseling services specifically designed for staff, promoting the importance of mental health in high-stress roles. 4. Setting Boundaries: It’s essential for nurses to recognize their limits and to take time off when needed. Establishing boundaries between work and personal life helps prevent burnout and maintains passion for their profession. Taking regular breaks and utilizing vacation time can rejuvenate nurses and enhance their well-being.
The role of a cardiac ICU travel nurse is undeniably demanding, requiring a unique blend of technical skill and emotional resilience. As these nurses navigate the complexities of caring for critically ill patients, they often face significant emotional challenges that can impact their well-being. However, by implementing effective self-care strategies and fostering connections with peers, they can manage these challenges and find fulfillment in their work. Ultimately, the emotional landscape of cardiac ICU travel nursing is a testament to the strength and compassion of those who choose this path. It is not merely a job; it is a calling that requires dedication, empathy, and an unwavering commitment to patient care. As the stories of these nurses unfold, it becomes clear that while the road may be fraught with challenges, the rewards—both for the nurses and the lives they touch—are immeasurable. By recognizing the emotional impact of their work and prioritizing self-care, cardiac ICU travel nurses can continue to provide exceptional care while nurturing their own mental health and personal well-being.
Cardiac ICU Travel Nurse
Hospitals with cardiac units, travel nursing agencies, and healthcare systems specializing in critical care
Core Responsibilities
Provide acute care for critically ill patients with cardiac conditions, including post-operative management and emergency interventions.
Monitor vital signs, administer medications, and collaborate with multidisciplinary teams to develop patient care plans.
Offer emotional support to patients and their families, helping them navigate the complexities of critical care situations.
Required Skills
Advanced knowledge of cardiac anatomy, physiology, and pharmacology.
Proficiency in using advanced medical equipment such as ventilators and cardiac monitors.
Strong communication skills to effectively relay patient information to healthcare teams and families.
Clinical Nurse Specialist (CNS) in Cardiology
Academic medical centers, specialized cardiac care units, and healthcare organizations involved in research
Core Responsibilities
Serve as an expert consultant in cardiology, providing guidance on complex cases and developing evidence-based protocols for patient care.
Educate nursing staff and other healthcare professionals on best practices in cardiac care and patient management.
Conduct research and participate in quality improvement initiatives to enhance cardiac care outcomes.
Required Skills
Master’s degree in nursing with a focus on cardiology or critical care.
Certification as a Clinical Nurse Specialist (CNS) with a strong understanding of cardiac pathophysiology.
Ability to analyze clinical data and implement evidence-based practices effectively.
Cardiac Rehabilitation Nurse
Cardiac rehabilitation programs, outpatient clinics, and hospitals with dedicated rehabilitation services
Core Responsibilities
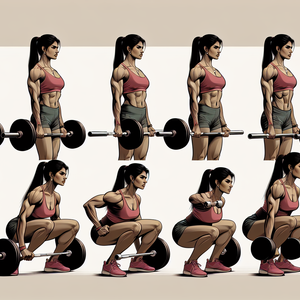
Develop and implement personalized rehabilitation programs for patients recovering from cardiac events such as heart attacks or surgeries.
Monitor patients’ progress, providing education on lifestyle changes, medication adherence, and exercise regimens.
Collaborate with cardiologists, physical therapists, and dietitians to ensure comprehensive care for each patient.
Required Skills
Strong background in cardiac nursing and patient education techniques.
Certification in cardiac rehabilitation (e.g., from the American Association of Cardiovascular and Pulmonary Rehabilitation).
Excellent interpersonal skills to motivate and support patients through their recovery journeys.
Critical Care Nurse Practitioner (CCNP)
Hospitals with ICU settings, specialty cardiac centers, and academic medical institutions
Core Responsibilities
Conduct comprehensive assessments and develop treatment plans for patients in the cardiac ICU, often working autonomously.
Perform procedures such as intubation, central line placement, and chest tube insertions as needed.
Lead and participate in family meetings to discuss patient progress and care decisions.
Required Skills
Doctorate of Nursing Practice (DNP) with a specialization in critical care or cardiology.
Advanced certification as a Family Nurse Practitioner (FNP) or Acute Care Nurse Practitioner (ACNP).
Strong decision-making skills and ability to work in fast-paced, high-stress environments.
Healthcare Mental Health Counselor for Nurses
Employee assistance programs (EAPs), healthcare institutions, and private counseling practices specializing in occupational therapy
Core Responsibilities
Provide mental health support and counseling tailored specifically for nursing professionals dealing with stress and compassion fatigue.
Conduct workshops and seminars on self-care strategies, resilience-building, and mental health awareness within the healthcare workforce.
Collaborate with healthcare organizations to develop programs aimed at improving staff wellbeing.
Required Skills
Master’s degree in counseling, psychology, or social work with a focus on healthcare settings.
Licensure as a mental health counselor or therapist, with experience in occupational mental health.
Empathy and understanding of the unique emotional challenges faced by healthcare providers.