The Human Touch in a Digital Age: Why Community Health Workers Will Always Be Indispensable

One of the key attributes that sets CHWs apart is their unparalleled emotional intelligence. Unlike AI, which relies on algorithms and data patterns, CHWs bring intuition, empathy, and personal experience to every interaction. They understand that healthcare is not just about clinical outcomes but also about addressing the emotional and psychological needs of patients. For example, a CHW working with a newly diagnosed cancer patient provides more than just information about treatment options. They offer a listening ear, a shoulder to lean on, and encouragement in moments of despair. Research shows that patients who feel heard and understood by their healthcare providers are more likely to adhere to treatment plans and experience better health outcomes. Machines, no matter how sophisticated, cannot replicate this deeply human connection.
Trust: The Foundation of Effective Healthcare
Trust is a cornerstone of effective healthcare, particularly in underserved or marginalized communities where systemic inequities often create barriers to care. Community Health Workers play a pivotal role in building this trust, as they are typically members of the communities they serve. Sharing cultural, linguistic, and socioeconomic backgrounds with their patients, CHWs bring a level of relatability and understanding that fosters confidence in the healthcare process. Consider a CHW working in an urban immigrant community. While an AI-powered chatbot might deliver health information in multiple languages, it cannot grasp the lived experiences that define the immigrant journey—fear of deportation, distrust of government systems, or the struggle to navigate a foreign healthcare system. A CHW, on the other hand, can approach patients with cultural humility, providing care that feels both respectful and relevant. This trust-building ability is irreplaceable and essential to ensuring equitable access to healthcare.
Cultural Competency in a Multicultural World
As societies become increasingly diverse, the demand for culturally competent healthcare has never been greater. Cultural norms, values, and beliefs significantly influence how individuals perceive health, illness, and treatment. CHWs, often drawn from the very communities they serve, are uniquely positioned to bridge the gap between Western medical practices and culturally specific health beliefs. Take, for instance, CHWs working with refugee populations. Refugees often face multiple barriers—language differences, trauma from displacement, and unfamiliarity with local healthcare systems. A CHW who shares their cultural background can act as a translator not just of words but of meaning, explaining medical concepts in ways that resonate with cultural traditions. AI, even with advanced translation capabilities, cannot grasp the intricate cultural contexts that CHWs navigate daily. This cultural competency is a vital part of ensuring healthcare is inclusive and effective for all.
The Limits of Technology in Addressing Social Determinants of Health
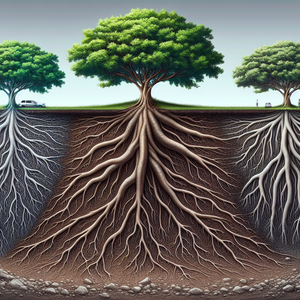
While AI excels in processing data, diagnosing diseases, and identifying trends, it falls short when addressing the social determinants of health—factors like income, education, housing, and access to nutritious food. These determinants often require a level of human insight and intervention that technology simply cannot provide. For example, imagine a single mother struggling to manage her child’s asthma. An AI system might generate a list of guidelines for asthma management, but it cannot identify the underlying challenges, such as her inability to afford medication or arrange childcare to attend doctor’s appointments. A CHW, however, can assess the situation holistically. By connecting her with local resources for financial aid, childcare, or transportation, the CHW addresses the root causes of the problem, enabling better health outcomes for the family. This nuanced, relationship-based approach is something no machine can replicate.
The Future: A Partnership Between Humans and Technology
As we look to the future, the relationship between CHWs and technology should not be seen as adversarial but collaborative. Rather than replacing CHWs, AI and automation can serve as powerful tools to enhance their work. For example, AI can help CHWs identify at-risk patients by analyzing large datasets, track community health trends, or streamline administrative tasks, freeing up CHWs to focus on building relationships and delivering care. In practice, this symbiosis is already emerging. AI algorithms can flag patients likely to develop chronic diseases, enabling CHWs to prioritize outreach to those individuals. Wearable health devices can provide real-time data on patients’ vital signs, which CHWs can use to tailor their interventions. By leveraging technology in this way, CHWs can amplify their impact while preserving the critical human touch that defines their role.
Will CHWs Persist in the Next Three Decades?
The rapid pace of technological innovation raises questions about the future of many jobs, including those of CHWs. However, while automation has replaced repetitive, task-based roles in other industries, the role of CHWs is fundamentally different. It is deeply relational, requiring emotional intelligence, cultural insight, and trust-building—qualities that machines cannot replicate. Consumer preferences also suggest a continuing demand for human-centered care. In an era where patients increasingly value personalized, empathetic interactions, the role of CHWs aligns perfectly with shifting societal expectations. Far from being made obsolete, CHWs are likely to become even more critical as healthcare systems strive to balance technological efficiency with human compassion.
In the digital age, where AI and automation are revolutionizing industries, the role of Community Health Workers remains as vital as ever. Their emotional intelligence, ability to build trust, and cultural competency are qualities that no machine can replicate. While technology can enhance their work by improving efficiency and providing actionable insights, it cannot replace the deeply human connection that CHWs bring to their communities. As the healthcare industry continues to evolve, it is clear that CHWs are not relics of the past but pioneers of a more inclusive, compassionate future. By combining cutting-edge technology with the irreplaceable human touch, we can create a healthcare system that addresses both the science and the soul of healing. In a world increasingly dominated by machines, the enduring value of CHWs reminds us that empathy, understanding, and trust will always be at the heart of healthcare.
Population Health Data Analyst
Hospitals, public health departments, nonprofit organizations, and health tech companies
Core Responsibilities
Analyze health data to identify trends and disparities within communities, enabling targeted health interventions.
Collaborate with healthcare providers and CHWs to translate data insights into actionable programs.
Assess social determinants of health through data visualization and geographic information systems (GIS).
Required Skills
Proficiency in statistical software (e.g., SAS, R, or Python) and data visualization tools (e.g., Tableau, Power BI).
Strong understanding of public health concepts and social determinants of health.
Ability to synthesize large datasets into meaningful insights for non-technical stakeholders.
Health Equity Program Manager
Nonprofit organizations, government health agencies, and healthcare systems
Core Responsibilities
Design and implement initiatives to address health disparities in underserved populations.
Partner with CHWs and community organizations to ensure programs are culturally relevant and effective.
Monitor program outcomes and report on progress toward equity goals.
Required Skills
Expertise in cultural competency and community engagement strategies.
Strong project management and grant-writing experience.
Familiarity with policy advocacy to address systemic barriers to health equity.
Digital Health Integration Specialist
Health tech startups, consulting firms, and hospital IT departments
Core Responsibilities
Train CHWs and other healthcare workers to use digital tools such as wearable devices, telehealth platforms, and AI-driven apps.
Adapt technology to meet the specific needs of diverse populations, ensuring accessibility and usability.
Troubleshoot issues with digital health tools and work with developers to address user feedback.
Required Skills
Experience with health technology platforms and familiarity with interoperability standards (e.g., HL7, FHIR).
Strong communication skills to bridge the gap between tech developers and end-users.
Background in healthcare or public health is a plus.
Behavioral Health Outreach Specialist
Community health centers, mental health organizations, and local governments
Core Responsibilities
Provide mental health education and outreach services tailored to specific communities.
Work closely with CHWs to identify individuals in need of behavioral health support and connect them to resources.
Develop culturally sensitive mental health programs that incorporate community feedback.
Required Skills
Training in mental health first aid, motivational interviewing, or trauma-informed care.
Deep understanding of cultural attitudes toward mental health in diverse populations.
Strong interpersonal skills to build trust and rapport with vulnerable individuals.
Social Determinants of Health (SDoH) Coordinator
Health insurance companies, accountable care organizations (ACOs), and public health departments
Core Responsibilities
Assess and address non-clinical factors affecting health, such as housing, food security, and transportation.
Partner with community organizations to connect individuals to resources that improve overall well-being.
Develop strategies to incorporate SDoH considerations into broader healthcare initiatives.
Required Skills
Knowledge of case management and resource navigation systems.
Ability to collaborate across sectors, including housing, education, and social services.
Experience with program evaluation and reporting outcomes to stakeholders.