The Therapeutic Alliance: Building Trust and Rapport as a PMHNP
At its essence, the therapeutic alliance is a collaborative partnership characterized by mutual respect, trust, and understanding between the PMHNP and the patient. Research consistently supports the notion that a robust therapeutic alliance leads to improved treatment outcomes, heightened patient satisfaction, and increased engagement in the therapeutic process. When patients feel understood and supported, they are more likely to share their feelings and experiences openly, allowing for more effective interventions and care.
Effective Communication Techniques
Effective communication serves as a cornerstone for building a solid therapeutic alliance. PMHNPs utilize various strategies to foster open dialogue and create a safe space for their patients. One of the most crucial skills in this context is active listening. By giving patients their full attention, acknowledging their emotions, and reflecting back what they say, PMHNPs demonstrate their genuine investment in their patients' well-being.
Empathy as a Cornerstone
Empathy is another essential component of the therapeutic alliance. PMHNPs who express genuine understanding and compassion create an environment where patients feel safe to explore their thoughts and emotions. This empathetic approach can significantly alleviate feelings of isolation and shame that often accompany mental health struggles.
Real-Life Examples of Successful Patient Interactions
Real-life examples of the therapeutic alliance in action can further illustrate its importance. Consider the story of a PMHNP who worked with a young adult struggling with severe depression. Initially, the patient was withdrawn and reluctant to engage in therapy. However, through consistent, compassionate communication and a focus on building trust, the PMHNP gradually helped the patient open up about their feelings and experiences.
In the field of psychiatric mental health, the therapeutic alliance is a critical factor that can profoundly influence the course of treatment. PMHNPs, through the use of effective communication techniques, the demonstration of empathy, and the cultivation of an environment of trust, can create meaningful connections with their patients. These relationships not only enhance treatment outcomes but also empower patients to take an active role in their healing journey.
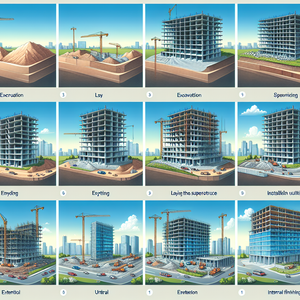
Psychiatric Mental Health Nurse Practitioner (PMHNP)
Behavioral health clinics, hospitals, and private practices
Core Responsibilities
Conduct comprehensive assessments and develop individualized treatment plans for patients with mental health disorders.
Utilize evidence-based practices to provide psychotherapy and medication management.
Foster strong therapeutic alliances through effective communication and empathetic engagement with patients.
Required Skills
Master’s degree in nursing with a focus on psychiatric mental health.
Active PMHNP certification and state licensure.
Proficient in crisis intervention techniques and patient advocacy.
Clinical Psychologist
Mental health clinics, hospitals, and academic institutions
Core Responsibilities
Provide psychological evaluations and therapeutic interventions for individuals facing mental health challenges.
Employ various therapeutic modalities, including cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT).
Collaborate with interdisciplinary teams to ensure comprehensive patient care.
Required Skills
Doctoral degree in psychology (Ph.D. or Psy.D.) and state licensure.
Strong analytical and critical thinking skills for interpreting psychological assessments.
Exceptional communication and interpersonal skills to build rapport with patients.
Licensed Clinical Social Worker (LCSW)
Social service agencies, hospitals, and mental health organizations
Core Responsibilities
Assess and diagnose mental health and emotional issues in clients, providing counseling and support.
Develop and implement treatment plans in collaboration with clients and other healthcare providers.
Advocate for clients’ needs within the healthcare system and connect them with community resources.
Required Skills
Master’s degree in social work (MSW) and state licensure as an LCSW.
Experience in trauma-informed care and crisis intervention.
Strong ability to navigate social systems and resources to support client well-being.
Psychiatric Nurse Specialist
Psychiatric hospitals, outpatient clinics, and rehabilitation centers
Core Responsibilities
Provide specialized nursing care for patients with psychiatric conditions under the supervision of psychiatrists or PMHNPs.
Monitor patients' progress and response to treatment, adjusting care plans as necessary.
Educate patients and families about mental health conditions and treatment options.
Required Skills
Bachelor’s degree in nursing (BSN) with specialized training in psychiatric nursing.
Strong observational skills and ability to assess patient behaviors and symptoms.
Excellent communication skills to engage effectively with patients and families.
Mental Health Counselor
Community mental health centers, schools, and private practices
Core Responsibilities
Provide individual and group counseling to clients dealing with mental health issues.
Develop personalized treatment strategies and support clients in achieving their therapeutic goals.
Facilitate workshops and support groups to promote mental health awareness and coping strategies.
Required Skills
Master’s degree in counseling or a related field and relevant licensure.
Knowledge of various therapeutic techniques and interventions.
Strong empathy and active listening skills to foster a supportive environment for clients.